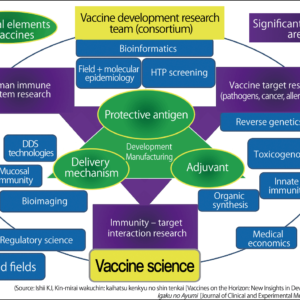
A weapon created to enable humanity to conquer infectious disease, vaccines have saved us from such terrible, life-threatening diseases as smallpox and polio. It would be fair to say that they are one of the most powerful tools of medical care, creating robust immunity throughout society. In fact, vaccines offer possibilities beyond the realm of infectious diseases. Scientists are already engaged in development research focused on vaccines to eliminate cancer cells and vaccines to tackle lifestyle-related diseases such as metabolic syndrome.
Special Feature 1 – The Past, Present, and Future of Vaccines A powerful weapon against infectious diseases —— Vaccines will save humanity
composition by Rie Iizuka
Vaccines first entered history more than 200 years ago, when one was used to protect people from the much-feared smallpox, a highly infectious disease with a mortality rate of 20-30%. The variola virus spread from person to person by airborne droplets or physical contact, causing many fatalities around the world. Although nobody at the time understood immune function or the fact that the disease was caused by a virus, people knew from experience that someone who had caught smallpox once never caught it again.
People infected with cowpox did not catch smallpox
The British physician Edward Jenner heard a dairymaid say, “I shall never have smallpox for I have had cowpox [a form of smallpox infecting cows].” With extraordinary insight, he embarked on research to see whether this fact could assist in preventing smallpox.
When a human catches cowpox, blisters form on their skin. Jenner extracted fluid from one of these blisters and injected it into a number of people, starting with James Phipps, his servant’s son. When, after repeatedly using this method, he eventually injected James and others with smallpox, none of them caught the disease. This is where vaccines originated and was the equivalent of today’s live vaccines.
Subsequent improvements and progress in scientific research led to people around the world being immunized with the live smallpox vaccine and in 1980, the World Health Organization (WHO) declared that smallpox had been eradicated worldwide. Painstaking studies and immunization drives were conducted until this outcome was reached. WHO staff traveled around world and went around showing people photographs of smallpox sufferers, asking whether they had seen any children with a similar disease. When the WHO staff found sufferers, they vaccinated everyone in the vicinity.
The last person infected with naturally occurring smallpox was found in Somalia in 1977. This is the only example of the acquisition of herd immunity on a global scale.
Incidentally, many Japanese biographies of great figures from history state that the first person Jenner vaccinated was his own son, but this is not a historical fact. Nevertheless, this does not detract from the achievement of this man, who wished to contribute to society as a whole, and did not seek a patent for his vaccination technique.
Derived from vacca, the Latin for “cow,” the word “vaccine” is believed to have been coined by Louis Pasteur. Pasteur believed that the vaccination technique could be applied to other infectious diseases and went on to develop various vaccines.
Emergency import of the polio vaccine and nationwide mass vaccination
Aside from smallpox, another vaccine that has had a major impact is the polio vaccine. Outbreaks of poliovirus infection began to spread in Japan in 1949 or thereabouts and more than 5,000 people were infected in 1960, primarily in Hokkaido. Most of the patients were aged five or under and quite a few were left with paralysis of the limbs or respiratory muscles.
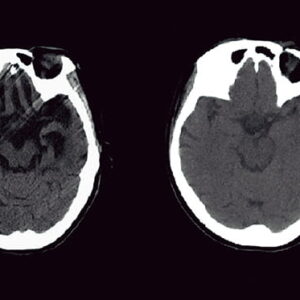
At the time, an inactivated polio vaccine (IPV) was used for vaccinations in Japan, but it was not sufficiently effective to bring the epidemic to a halt. Patients with respiratory failure were placed in an “iron lung” —— a large ventilator enclosing the body —— but quite a few children lost their lives because there were not enough of these devices to go around.
To overcome this grave situation, the Minister of Health and Welfare at the time, Yoshimi Furui, decided to order the emergency import of the live oral polio vaccine (OPV) from Canada and Soviet Union (now Russia) in the midst of the Cold War, so that a nationwide program of mass vaccination could be carried out. It was tremendously effective, and the number of people infected fell almost to zero the following year (Figure).
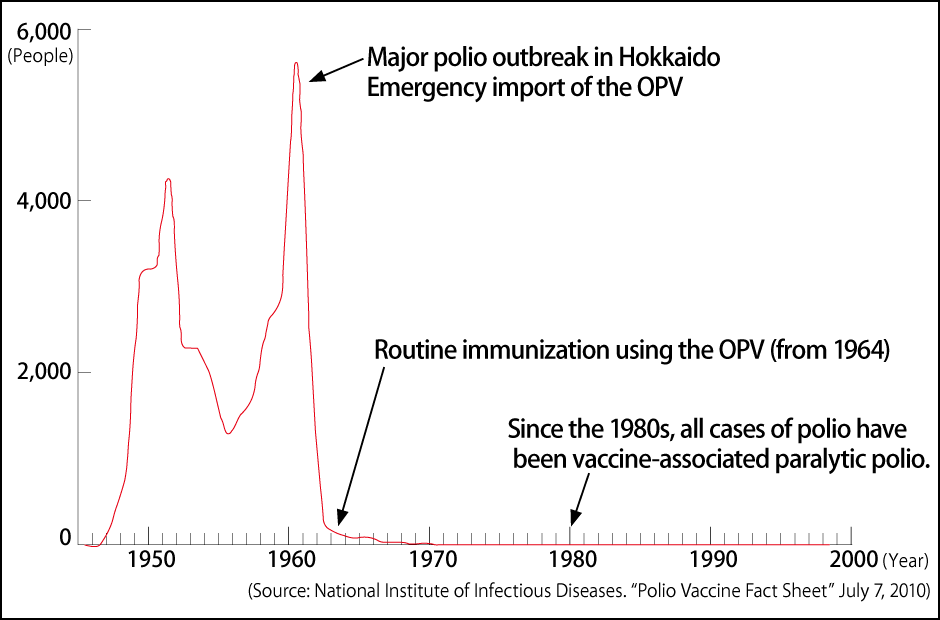
Figure. Polio cases in JapanPolio began to sweep Japan in the 1940s and more than 5,000 patients were counted people were infected with the disease across the country in 1960, but the OPV imported into the country on an emergency basis had a groundbreaking effect. There have been no cases of polio in Japan since the last one in 1980.
As the live polio vaccine is administered orally and creates immunity through the proliferation of the attenuated virus in the intestines, there was a risk that others might be infected via feces. Accordingly, mass vaccination was carried out within a short period at designated vaccination centers in each area to prevent secondary infection caused by people already vaccinated. In addition to the effects of the live vaccine, it was the adoption of an appropriate approach to vaccination that led to the eradication of polio in Japan. In making this bold decision, Minister Furui reportedly said, “I will take full responsibility.” I believe that he bequeathed a truly great achievement to us.
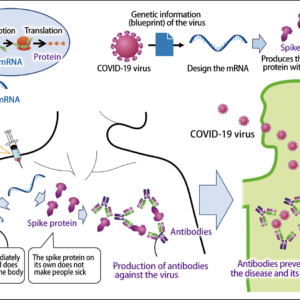
Vaccines are broadly divided into two categories: live vaccines and inactivated vaccines. Live vaccines are made from pathogenic viruses or bacteria whose pathogenicity (virulence) has been extremely weakened, so the virus or bacterium in question is not dead. Various methods are used to adjust the virulence, such as drying the pathogen or repeatedly culturing it hundreds of times. After vaccination, the virus proliferates in the body and our immune function starts working to counteract it, thereby enabling us to gain immunity. As the immunity gained is powerful, the vaccine does not need to be administered many times and even babies’ immature immune systems can acquire robust resistance. However, as the vaccinated individual is what might be termed mildly infected, a gap of four weeks is required before giving them any other vaccine. In rare cases, people can suffer a side effect in the form of mild clinical symptoms.
Inactivated vaccines use pathogens that have had their infectivity eliminated (dead pathogens) and some inactivated vaccines require a very large quantity of antigen compared with live vaccines. As their mechanism for providing immunity is weaker than that of live vaccines, multiple vaccinations are required.
There is a misperception of live vaccines as old and primitive, and inactivated vaccines as advanced. The rotavirus vaccines launched in 2011 and 2012 are highly effective orally administered live vaccines and were added to Japan’s routine vaccination schedule in FY2020. Live vaccines create immunity in an extremely similar way to natural infections and can be introduced into the body via a natural means, such as orally or via nasal drops. It is not a matter of live vaccines being better than inactivated vaccines or vice versa; rather, their distinctive features are leveraged to ensure that the right form is used for the right purpose.
Swelling or a mild fever is a normal reaction after a vaccination
The existence of side effects is thought to contribute to vaccine hesitancy. As vaccines use human immune function to confer resistance, it would be fair to say that developing swelling or a mild fever after a vaccination is a perfectly normal reaction. However, it is only natural that people feel nervous, because these reactions occur in otherwise healthy individuals as a result of being vaccinated. Each person’s physical makeup is different, so side effects present themselves in varying ways, too. My advice would be for people to remain calm, bearing in mind that immune reactions occur in response to vaccination and that some changes in physical condition might emerge.
Having said that, a vaccination method will need to be reviewed if symptoms not normally experienced as a result of the infection develop, such as acute encephalopathy or seizures. Currently, cases of anaphylactic shock due to COVID-19 vaccines are attracting attention, but as anaphylaxis does not occur in cases of COVID-19 infection, it would be hard to describe this as a normal immune reaction. Ingredients in the vaccine are among the several conceivable reasons for anaphylaxis, but information available at this point in time (April 12, 2021) indicates that the incidence is particularly high in Japan, with 1 case of anaphylaxis per 12,000 vaccinations, as opposed to 1 in 200,000 in the U.S.
While I am sure that any causal relationship will be explained in due course, great caution will be required in scaling up vaccinations going forward, with conceivable measures including putting in place medical systems capable of dealing with severe acute reactions. The use of vaccines should normally be approved on the basis of a cautious assessment of everything up to long-term impacts. In the case of COVID-19, I believe that the vaccines being used at present offer adequate advantages when considered in light of the balance of pros and cons amid this emergency.
Even where side effects do occur, some are likely to be down to an individual’s innate physical predisposition emerging, triggered by the vaccination. One cannot deny the possibility that a person’s anaphylaxis might one day have occurred in some situation, even if not as a result of the vaccine. However, efforts should obviously be made to avoid such anomalous immune reactions being triggered by vaccines.
Ideally, scientists would develop highly effective vaccines without side effects, but in reality, this is virtually impossible. Vaccines have been developed with consideration for their long-term impact, pursuing a balance between the maximum effectiveness and the minimum side effects.
There was a time when Japan was regarded as having a vaccine gap —— that is to say, it lagged behind other nations in its use of vaccines. However, a number of vaccines have since been added to the routine vaccination schedule, starting with Streptococcus pneumoniae (in children) in FY2013 and followed by Haemophilus influenzae type b (Hib), chickenpox, hepatitis B, and rotavirus (Table). This has gone a long way to closing the vaccine gap. However, a number of problems peculiar to Japan still remain, including the restoration of the mumps vaccine to the regular vaccination schedule and the fact that administration of the human papilloma virus (HPV) vaccine has effectively been suspended.
| WHO-recommended immunizations | Public immunizations in Japan | UK | U.S.A. | Germany | France | Italy | Canada |
|---|---|---|---|---|---|---|---|
| Recommended for all regions | |||||||
| BCG (tuberculosis) | ○ | △ | × | × | △ | × | × |
| Polio | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| DPT (D: diphtheria, P: pertussis (whooping cough), T: tetanus) | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| Measles | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| Rubella | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| Hepatitis B | ○ (added to the routine vaccination schedule in October 2016) |
○ | ○ | ○ | ○ | ○ | ○ |
| Hib (Haemophilus influenzae type b) | ○ (added to the routine vaccination schedule in FY2013) |
○ | ○ | ○ | ○ | ○ | ○ |
| Streptococcus pneumoniae (in children) | ○ (added to the routine vaccination schedule in FY2013) |
○ | ○ | ○ | ○ | ○ | ○ |
| HPV (human papilloma virus) | ○ (added to the routine vaccination schedule in FY2013) |
○ | ○ | ○ | ○ | ○ | ○ |
| Rotavirus | ○ (added to the routine vaccination schedule in FY2020) |
○ | ○ | ○ | × | ○ | ○ (administered in 12 of 13 provinces and territories) |
| Recommended for particular regions | |||||||
| Japanese encephalitis | ○ | × | × | × | × | × | × |
| Recommended to be administered on the basis of national immunization programs | |||||||
| Mumps | × | ○ | ○ | ○ | ○ | ○ | ○ |
| Chickenpox | ○ (added to the routine vaccination schedule in October 2014) |
△ | ○ | ○ | × | ○ | ○ |
| Influenza | ○ | ○ | ○ | ○ | ○ | ○ | ○ |
| Other (no WHO recommendation) | |||||||
| Streptococcus pneumoniae (in adults) | ○ (added to the routine vaccination schedule in October 2014) |
○ | ○ | ○ | × | ○ | ○ |
Table. Vaccinations in Japan and overseas* Recommended for people of all ages in the U.S., but only for elderly people elsewhere.
○: Administered as public immunizations (routine vaccinations in Japan)
×: Not administered (currently under evaluation)
△: Administered only to high-risk individuals
(Survey by the Health Service Bureau, Ministry of Health, Labour and Welfare, current as of the end of March 2019. Information on the rotavirus vaccine has been updated.)
While the vaccine gap is in the process of being eliminated, issues still remain, such as the inclusion of the mumps vaccine in the routine vaccination schedule.
Whenever the subject of vaccines comes up, I get asked, “They say that the influenza vaccine has no preventive effect because it’s a different type, but should I get vaccinated anyway?” The fact is that the effectiveness of vaccines in preventing infection varies widely, from vaccines such as smallpox and measles, which are virtually 100% effective, to those such as influenza, which require annual immunization and still could potentially allow an individual to become infected.
The influenza virus by its nature mutates very easily. The influenza vaccine is developed based on projections of the strain expected to circulate that year, but if a different type emerges, the vaccine’s effectiveness is limited. To ensure as great an effect as possible, each year’s vaccine is manufactured on the basis of the influenza virus strain that was circulating in the Southern Hemisphere six months earlier.
A virus cannot survive if it becomes prevalent and many people therefore develop antibodies to it. Accordingly, it is fair to say that once a virus reaches a certain level of prevalence and the number of people with antibodies increases, a mutated strain will inevitably emerge. The same applies to COVID-19.
The possibilities of vaccines go beyond infectious diseases
The organs infected and the cells that can be invaded differ from one virus to another. The influenza virus proliferates in the epithelial cells of the upper respiratory tract and does not enter the bloodstream. As there are many immune cells in the blood, the influenza virus proliferates in the upper respiratory tract, where the immune system cannot easily resist it. Given this characteristic of the influenza virus, the purpose of the vaccine is to prevent the disease progressing to pneumonia or other serious conditions, rather than to prevent infection itself.
HPV is another virus that does not enter the bloodstream, but rather proliferates in the epithelial cells, making it hard to acquire immunity, so the aim of the vaccine is to achieve a preventive effect somewhere in the region of 70%. Countermeasures vary according to the nature of the virus, with some vaccines able to achieve 100% elimination of the infections they cause, while in other cases, an effectiveness of 70-80% is enough.
At the same time, therapeutic drugs are also key to suppressing outbreaks of infectious diseases. Used in tandem, prevention and treatment can achieve major progress in combating infectious diseases. In the case of COVID-19, vaccines have come first, but there are ample reasons to expect that highly effective drugs to treat the disease will be developed, as they were for influenza.
Today, vaccines are mainly used for preventing infectious diseases, but scientists are already engaged in development research focused on vaccines to eliminate cancer cells and vaccines to tackle lifestyle-related diseases such as high blood pressure. I believe these vaccines will still face quite a few hurdles before they are commercialized, but the possibilities offered by vaccines will open up. In my view, vaccines will be called upon to play a wide range of roles in the future.