Vaccines are powerful weapons that save humanity from many infectious diseases. However, vaccine hesitancy is still deeply rooted in Japan, and more than 2,800 women a year die of cervical cancer, for example. Just as all drugs have side effects, there are no vaccines with no adverse reactions. Not every event that occurs after a vaccination is necessarily an adverse reaction. We must be fully aware of this and make appropriate judgments, taking into consideration the risks of infections.
Special Feature 1 – The Past, Present, and Future of Vaccines Risks from infectious diseases and adverse events following immunization
composition by Rie Iizuka
illustration by Koji Kominato
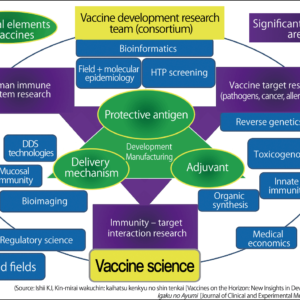
Vaccines are biological preparations whose purpose is to prevent infectious diseases and other conditions. A great deal of time and knowledge has gone into their development. Being vaccinated enables us to acquire immunity against a pathogen, in the expectation that this will be effective in preventing the onset or exacerbation of disease or death if that pathogen later enters the body. Vaccines also play a part in warding off the development of cancers caused by viruses and in preventing pregnant women from catching infectious diseases that could affect their unborn children. The biggest achievement by a vaccine to date is the eradication of smallpox, and vaccines as a whole are very useful drugs that save us from many other infectious diseases.
Adverse events, misattributed side effects, and adverse reactions
Let us assume that you have bought some medicine because you have caught a cold. Whether prescription medication or over-the-counter drugs, all medicines come with a sheet explaining the usage and dosage, and also listing the side effects that could potentially occur, such as “May cause drowsiness —— do not drive after taking” and “May cause a dry mouth —— drink plenty of water.” In fact, it would probably be fair to say that there are no medicines that do not come with a list of side effects. The same can be said for vaccines, which are a type of biological preparation.
Undesirable reactions of various kinds can occur after being vaccinated; these are divided into “adverse events,” “misattributed side effects” and “adverse reactions” (Figure 1).
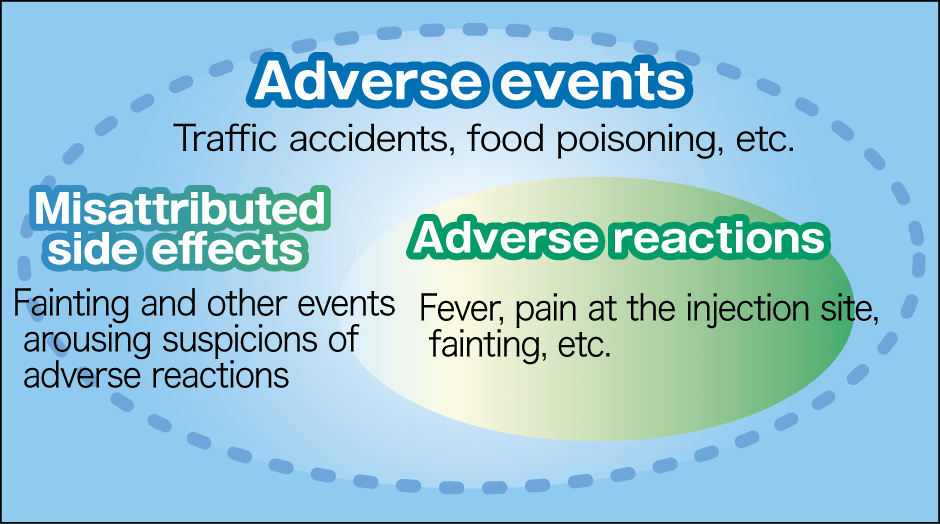
Figure 1. Adverse events, misattributed side effects, and adverse reactionsAdverse events are undesirable events that occur within a certain period after being vaccinated. They include both adverse reactions of the vaccine and misattributed side effects arousing suspicion that they might be an effect of the vaccine, but actually are not. A traffic accident on the way home from being vaccinated is an adverse event, but not an adverse reaction. On the other hand, fever after a vaccination is both an adverse event and an adverse reaction.
Adverse events are undesirable events, including coincidences, that occur after a vaccination, regardless of whether or not there is a causal relationship to the vaccination. For example, even a traffic accident on the way home from being vaccinated would be deemed an adverse event. After a vaccination, adverse events that are unrelated to the vaccination, but which make people want to suspect a connection are sometimes misattributed to the vaccination. One such example is the sudden infant deaths that became the focus of debate when the Hib vaccine and pneumococcal vaccine were added to the routine vaccination schedule. As no causal relationship has been found between the vaccination and sudden deaths, use of the vaccine has now resumed.
Adverse events such as rashes and fever that are thought to be the result of vaccination are called adverse reactions.
Japan has the Relief System for Injury to Health with Vaccination, which provides generous benefits to those whose health is affected by approved vaccines on the routine vaccination schedule unless the health problem is categorically proven not to have resulted from the vaccine. It would be fair to describe this as a world-class compensation that ensures people can enjoy peace of mind about being vaccinated.
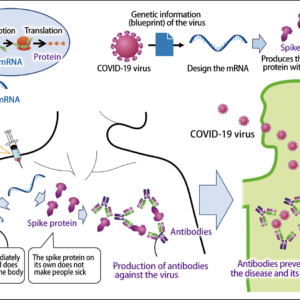
In the case of the new COVID-19 vaccines, adverse reactions including pain and swelling at the injection site, general malaise, and anaphylaxis have been reported in countries that began vaccinating people before Japan, but all those who have experienced such adverse reactions have recovered.
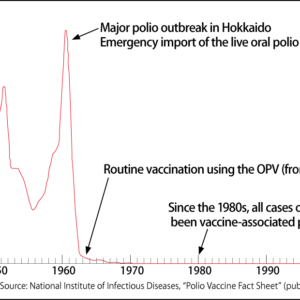
It is certainly true that problems have occurred with vaccines in the past. In the U.S. in 1955, a number of vaccinated children developed polio and some died, because a supposedly inactivated polio vaccine was contaminated with wild poliovirus.
In Japan in 1989, aseptic meningitis, whose symptoms include fever, vomiting, and headache, was found to have occurred at rates as high as 1 person in 933 following the administration of MMR vaccine. The MMR vaccine at the time combined measles, mumps, and rubella vaccines, so that they could be administered in one go, but the mumps vaccine component caused a large number of cases of aseptic meningitis after vaccination. It was subsequently discovered that part of the mumps vaccine manufacturing process had been altered. As a result, administration of the MMR vaccine as part of the routine vaccination schedule was halted in April 1993, since when a combined measles and rubella (MR) vaccine that does not contain the mumps vaccine component has been used for the routine vaccination program in 2006.
However, aseptic meningitis occurs in 3-10% of cases of natural mumps infection, and around 1 in every 1,000 people who develop the disease are left with aftereffects such as hearing loss. In the case of males who have reached puberty, 20-40% develop orchitis (inflammation of the testes). Orchitis causes a high fever and severe pain.
Major mumps epidemics occur in a four-to-six-year cycle, with the most recent occurring in 2009-2011 and 2015-2016. According to a survey by the Oto-Rhino-Laryngological Society of Japan, more than 300 people (with schoolchildren the worst affected, followed by people in the age bracket likely to have young children) were unfortunately left with hearing loss after the 2015-2016 epidemic. The incidence of aseptic meningitis due to the mumps vaccine is currently thought to be about one case in tens of thousands of people. However, Japan is the only developed country that still does not include the mumps vaccine in its routine vaccination schedule. We are currently gathering further evidence, with the aim of eliminating this situation.
Low rates of cervical cancer vaccination are a problem
Another problem is the low rate of vaccination with the human papillomavirus (HPV) vaccine, which prevents cervical cancer. In countries where it is part of the routine vaccination program, a decline in the onset of cervical cancer has recently been reported, but according to the 2018 Vital Statistics in Japan, more than 2,800 women per year in our country are still dying of cervical cancer. Immediately after routine vaccinations began, there were media reports of a diverse array of symptoms, including chronic pain and motor dysfunction, and vaccination rates fell, because of a lack of active encouragement to get vaccinated. However, large-scale studies carried out in Japan and overseas have shown no difference between vaccinated and unvaccinated people in regard to the symptoms of which people complained.
One adverse reaction of vaccination that can occur regardless of vaccine type is anaphylaxis. Additives used in the manufacture of vaccines are one cause of this. The 1990s saw many cases of allergic reactions caused by the gelatin used as a stabilizer in vaccines, but although it is still used in some vaccines overseas today, gelatin has been eliminated from all vaccines manufactured in Japan, at the very least. Adverse reactions whose cause has been clearly identified are dealt with properly when they arise, and the knowledge gained is applied in subsequent vaccine development.
Other vaccine ingredients known to cause allergic reactions include polyethylene glycol and polysorbate. While some of these preparations are used in COVID-19 vaccines, they are also used in such everyday products as cosmetic foundations and laundry detergents. In other words, some allergic reactions resulting from vaccinations stem from various materials in the vaccines. As information about vaccine ingredients is publicly available, we can check beforehand to see if a vaccine contains anything likely to cause us to experience an allergic reaction.
The vasovagal reflex is cited as another vaccine adverse reaction, but this occurs in as much as 1% of all instances of drawing blood or normal injections, not only vaccinations. Sometimes people’s feelings, such as fears or concerns about pain cause them to faint or feel unwell, but even these abate after resting for 30 minutes. People in whom such reactions have previously been observed receive their vaccinations lying down on a bed.
At the same time, live vaccines can cause symptoms that are similar to, but milder than the disease itself. Live vaccines undergo a process called attenuation, which involves eliminating almost all of the virus’s virulence, while maintaining its properties in order to trigger an immune response. This is why humans sometimes present the symptoms distinctive of the infectious disease in question.
For example, around 20% of people who receive the measles vaccine develop a fever and a slight rash about a week after vaccination. It usually resolves itself within a day or two, but if you have a high fever or severe symptoms, you should see a doctor. While this is an adverse reaction of the vaccine, the physician who supervised my laboratory at the university used to say, “That should be called a clinical response, rather than an adverse reaction.” In other words, developing a fever or rash to some degree is an ordinary foreseeable reaction due to the nature of the measles or rubella virus.
Vaccine hesitancy is regarded as being stronger in Japan than overseas. The cautious nature of Japanese people is perhaps one factor behind this, but I believe we need to anticipate what kind of reactions could occur when being vaccinated.
When I worked as a pediatrician, I made a point of not telling the children I was about to vaccinate that it would not hurt. Of course, injections hurt. That is why I told them, “It might hurt a bit, but only a little, so be brave.” I also told their parents or guardians about the kind of reactions that could occur, depending on the nature of the vaccine. For instance, I told them, “The site of the injection might swell, and they might develop a fever in about a week, so avoid any travel then.” Managing expectations in this way should go some way to easing anxiety about receiving something unknown.
Being vaccinated when not unwell might give rise to vaccine hesitancy, but I want people to know how beneficial vaccines are.
If a pregnant woman is infected by rubella viruses before she is past the 20th week or so of her pregnancy, her baby is at risk of developing a disability called congenital rubella syndrome, which causes heart disease, hearing loss, and cataracts. Rubella is a disease that must not be treated lightly, as it can also cause encephalitis (reported in about 1 in every 1,800 people during the 2018-2019 epidemic) and thrombocytopenic purpura (reported in about 1 in 250 people in the same epidemic).
In 2015, based on the results of vaccination of men and women alike from an early stage, the Region of the Americas was declared by the World Health Organization (WHO) to have eliminated rubella. Japan, on the other hand, began routine rubella vaccination of female junior high school students in 1977, but following various complications, now recommends routine vaccination of boys and girls alike in two stages: one dose at age one and the second at age five or six. However, as men born between April 2, 1962 and April 1, 1979 did not have the opportunity to undergo routine vaccination, a higher percentage of them have no antibodies compared to other age groups. This means that, if a person catches rubella, the infection spreads mainly within that age group, which can have a major impact not only on the individuals infected, but also on those around them.
In fact, there was a nationwide rubella epidemic in 2012 and 2013, with as many as 16,730 cases reported to the Ministry of Health, Labour and Welfare over the two-year period. The babies of 45 women infected while pregnant developed congenital rubella syndrome. The outbreak was centered exactly on men in the age group that had not had the opportunity to undergo routine vaccination (Figure 2).
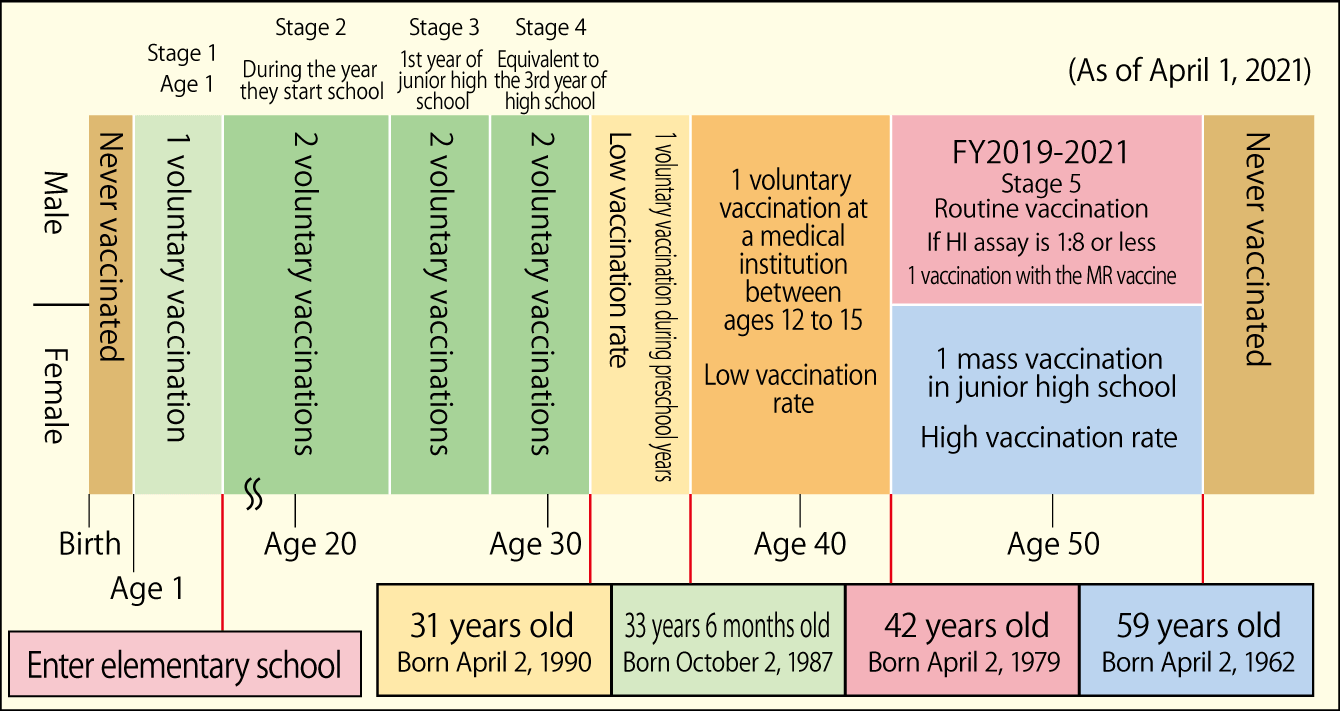
Figure 2. MMR/MR vaccinations, legal changes and age groupsAntibody levels vary due to changes in the vaccination administration. Men aged between 42 and 59 as of April 1, 2021 have few antibodies, because they had no opportunity to receive the rubella routine vaccination.
As the same situation arose at the time of the 2018-2019 epidemic (Figure 3), a temporary measure is now in place, under which approximately 15 million men in the age group that did not have the opportunity to undergo routine vaccination can receive a rubella antibody test and, if their antibody titer is low, can receive the MR vaccine free of charge. This program began in 2019, and men in the age bracket in question should have received a notice about it from their local government. However, although two years have already passed since then, only about 19% of those eligible have actually taken the antibody test.
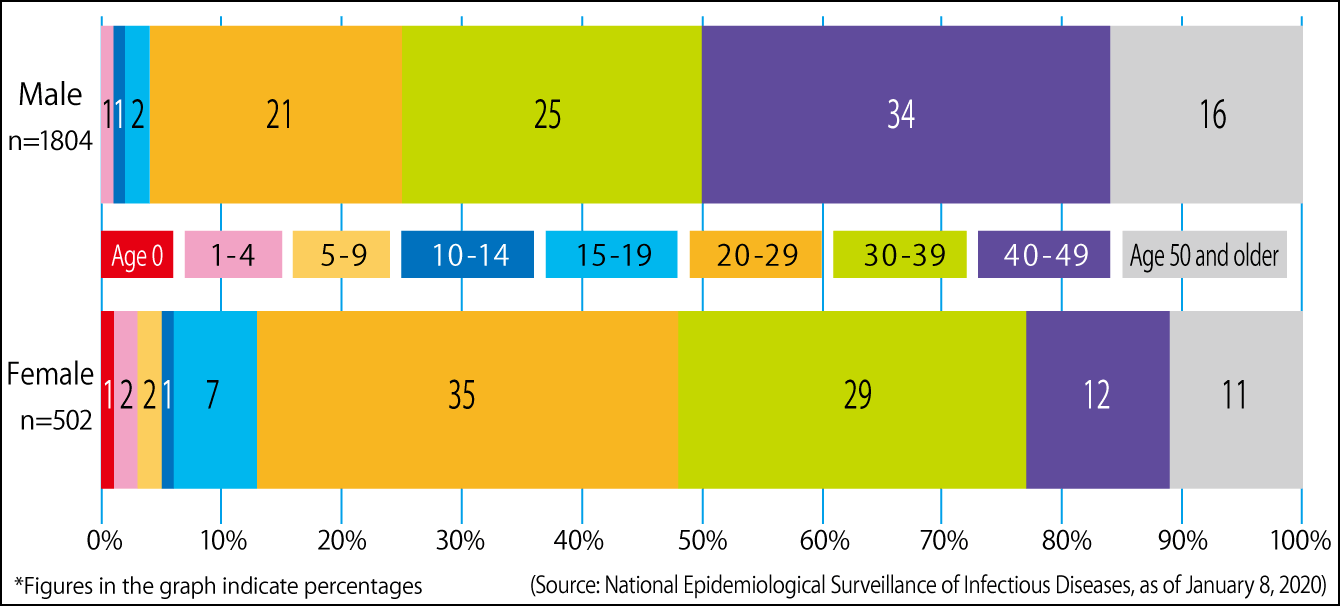
Figure 3. Proportion of individuals infected with rubellaIn the 2019 epidemic, 94% (2,176 people) of those reported as infected were adults, with 3.6 times as many men as women (1,804 men, 502 women) infected. Of particular note was the fact that men in their 30s and 40s accounted for 59% of all men infected. Many of the women who caught the disease (64% of all women infected) were of childbearing age (in their 20s and 30s).
Vaccines can curb severe impacts
Symptoms of rubella develop following an incubation period of two to three weeks after infection, but as an individual infected with rubella is contagious for a week before they become symptomatic, there is a not insignificant possibility that they could infect a pregnant woman without realizing it. It is so serious that the U.S. has warned pregnant women without rubella antibodies to refrain from traveling to Japan. The reality of infectious diseases is that even if one’s own symptoms are mild, they could have a severe impact on someone else. Accordingly, I want people to understand that vaccines can mitigate that risk.
Looking back 20 years, the vaccination rate of one-year-olds with the MR vaccine was around 50%. Hundreds of thousands of children caught rubella and dozens died. Wanting to do something about that, we organized a campaign under the slogan “Make your child’s first birthday present the MR vaccination.” No parent or guardian wants to give a child their first birthday present on their second birthday. What we were saying was that we wanted people to have their children vaccinated as soon as they became one year old. Now, 20 years on, the vaccination rate is more than 95%, and Japan is verified as having eliminated measles. Of course, we cannot afford to let our guard down, as the disease can still be brought in from overseas, but it is a positive example that demonstrates how vaccines can prevent disease.

As stated at the beginning, vaccines are a biological preparation. Just as all drugs have side effects, there are no vaccines with no adverse reactions. The symptoms that occur after vaccination are a mixture of those that have a clear causal relationship to vaccination and those that do not. I hope that you will make the right choice, understanding both the events that can occur after vaccination and the risks you face if you are infected.