Scientists have long known about the gut–brain axis —— the network linked by the vagus nerve that allows the brain and the gut to exchange information and influence each other via hormonal interactions. In recent years, it has become apparent that gut microbes are closely involved in this process. This raises questions about their relationship to diseases of the brain. Attention is focusing in particular on the connection to dementia. At the National Center for Geriatrics and Gerontology (NCGG)’s Center for Comprehensive Care and Research on Memory Disorders, scientists began researching the relationship between gut microbes and dementia in 2016. These studies have brought to light lifestyle habits that can assist in prevention.
Special Feature 1 – Forefront Research into Gut Bacteria Gut microbiomes and cognitive function
composition by Toshiko Mogi
It is said that around one in three elderly people aged 65 or above in Japan suffers from either dementia or mild cognitive impairment (a state in which an individual does not have dementia, but does have lower cognitive function than previously). Dementia is a condition in which cognitive function (mental faculties such as memory, thinking, calculation, judgment, and language) is reduced by various diseases or other causes, thereby interfering with daily life. As is true of all diseases, early detection and treatment are key. In the case of dementia, too, it is vital to identify and address the condition as soon as possible.
Research flourished after the introduction of next-generation sequencers
The NCGG’s Center for Comprehensive Care and Research on Memory Disorders, where I work, is a medical center specializing in dementia. The Center has both an out and inpatient department. The outpatient department aims to ensure early diagnosis of patients with memory disorders and the provision of appropriate treatment.
The impetus for patients seeking treatment from us varies: sometimes it is the individual themselves who initiates the consultation, after developing misgivings that they might have dementia due to forgetting things more frequently; sometimes spouses attend a consultation together, so that the individual suspected of having dementia will be be more encouraged see a physician; and sometimes concerned family members will bring an elderly patient living alone to a consultation. Judgments on the cognitive functions of the patients who come to see us can be broadly divided into three categories: normal (subjective cognitive impairment only); mild cognitive impairment (pre-dementia); and dementia.
As the relationship between various diseases and gut microbes has become the focus of attention in recent years, research is progressing in various fields. The connection via which the brain and gut influence each other is called the gut–brain axis. How are the brain and gut connected, when they are so far apart? The answer to this question is still being unraveled. Research in this realm began to flourish when next-generation sequencers capable of decoding genome sequences at high speed appeared. Partly because of these background developments, our research team thought that there might also be a connection between gut microbes and dementia, so, after obtaining the consent of outpatients visiting our memory clinic, we embarked in 2016 on a study of the relationship between the gut microbiome and dementia.
We conducted the study by means of the following procedure. We first conducted psychological tests and MRI scans on outpatients visiting our memory clinic who had given consent to participate in the study. The purpose of these tests and scans was to determine whether or not they had dementia. Next, we obtained fecal samples from the patients, which were analyzed by a laboratory testing company. The purpose of this was to understand the state of patients’ gut microbes from their feces, as there are approximately 100 billion gut microbes in 1 g of feces. The clinical and laboratory testing data thus obtained was anonymized and managed in the hospital’s biobank (research data management system). We then integrated our research data and, with the cooperation of other research institutions, conducted analysis that incorporated medical, scientific, and statistical perspectives, among others.
Gut microbes are strongly associated with cognitive decline
The bacteria that reside in the gut cluster together by species and cling to the intestinal wall, covering it completely. The formal name for what is often referred to as gut flora is the gut microbiome.
A 2011 article states that the human gut microbiome can broadly be classified into three enterotypes by diet and lifestyle, unrelated to sex or race. Gut microbiomes in which Bacteroides is the dominant genus of gut microbes are classed as enterotype I, those in which Prevotella is predominant are categorized as enterotype II, and those in which Ruminococcus or other microbes are the main genus are classified as enterotype III.
The first study we conducted explored the relationship between these enterotypes and dementia. With the cooperation of 128 patients aged in their 60s to 80s, we conducted the study described above. Of these patients, whose mean age was 74, 34 had been diagnosed with dementia, while the remaining 94 had not.
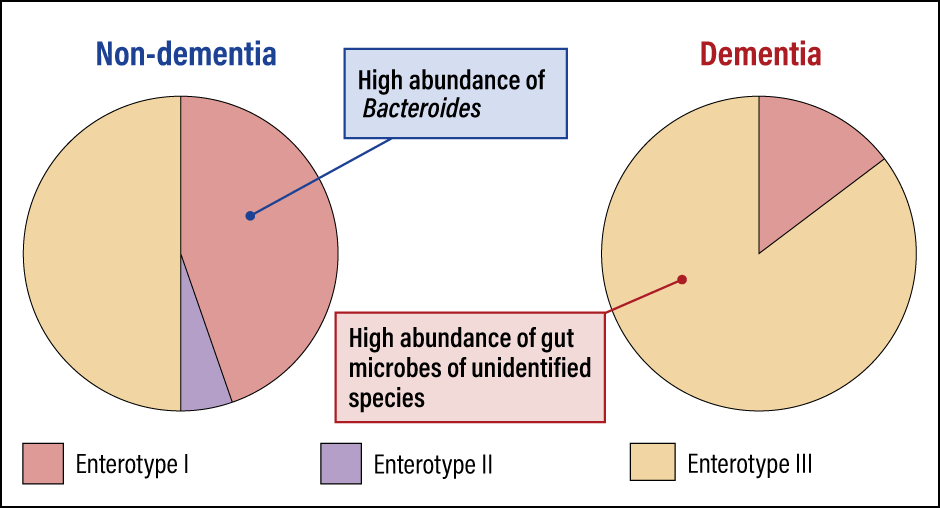
When we compared the results for the patients with dementia and those for the patients without, we found their enterotypes differed (Figure 1). The proportion of enterotype I in those with dementia was low, while the proportion of enterotype III was high.
 Modified from Saji N, et al. Sci Rep, 9(1):1008, 2019.
Modified from Saji N, et al. Sci Rep, 9(1):1008, 2019.
Figure 1. Enterotypes differ according to whether or not dementia is presentIn the non-dementia group, 45% of individuals had enterotype I microbiomes, with a high abundance of Bacteroides. However, in the dementia group, enterotype I microbiomes were found in just 15%, whereas 85% had enterotype III, with a high abundance of gut microbes of unidentified species.
We also discovered that the tendency of people with enterotype I to have dementia was lower than individuals in whom other bacteria were prevalent, at just one-tenth of the level. When we published these findings as an article in January 2019, it created a major sensation, and our article was selected as one of the top 100 in the journal in which it was published.
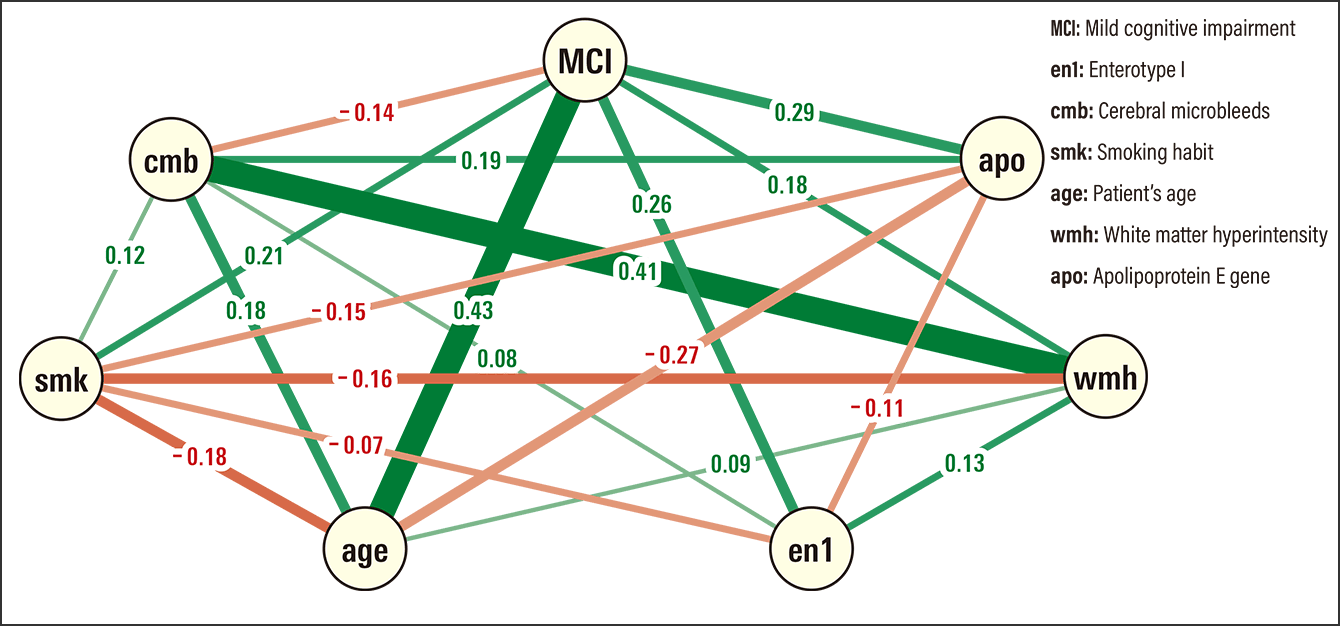
Thus, we obtained the new finding that the gut microbiome differs substantially according to whether or not an individual has dementia, but the relationship between mild cognitive impairment —— the stage prior to dementia —— and gut microbes remained unclear. Accordingly, in our next study, we investigated people who did not have dementia and discovered that gut microbes are also strongly associated with cognitive decline in cases of mild cognitive impairment (Figure 2).
 Modified from Saji N, et al. Sci Rep, 9(1):19227, 2019.
Modified from Saji N, et al. Sci Rep, 9(1):19227, 2019.
Figure 2. Gut microbes change at the pre-dementia stageLine thickness indicates the strength of the association, with green lines indicating a positive relationship and red lines a negative one. There is a positive relationship between mild cognitive impairment (MCI) and gut microbes (en1). Changes in gut microbes increase the risk of mild cognitive impairment roughly fivefold, indicating that changes in gut microbes occur before dementia onset.
Of the 82 patients without dementia on whom the study focused, 61 were diagnosed as being in the mild cognitive impairment group and these subjects had more enterotype I microbes than those with normal cognitive function. In addition, brain MRI scans revealed a large number of abnormal findings among patients in this group, in the form of white matter hyperintensity in the cerebrum, and they also had a high level of hippocampal atrophy.
Furthermore, even when we adjusted for known dementia risk factors using multivariate analysis, we found no relationship to risk factors such as age and sex, but discovered that changes in gut microbes increased the risk of mild cognitive impairment roughly fivefold.
The following three characteristics emerge from this series of results.
- Individuals who developed dementia have a high abundance of microbes of unidentified species (enterotype III).
- Bacteroides is the dominant genus (enterotype I) in individuals with mild cognitive impairment —— the stage prior to dementia.
- The enterotype does not change as dementia progresses; rather, these results show the characteristics of the gut microbes at each level of dementia progression.
These characteristics show a strong association between dementia and gut microbes, and that changes begin to occur in the gut microbiome before dementia onset.
Do metabolites affect dementia?
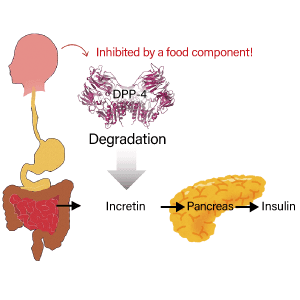
While we have discovered that there is a strong association between cognitive function and gut microbes, the mechanism explaining why gut microbes are associated with cognitive function remains unclear. Accordingly, the next thing we focused on was the metabolites produced by gut microbes.
A large, diverse array of metabolites are produced by gut microbes in the process of metabolizing the nutrients that reach the colon. The metabolites differ according to the content of the individual’s diet and the microbes living in their gut. Among these metabolites are the likes of butyric acid and acetic acid, which have the positive effect of curbing the proliferation of harmful microbes and the generation of putrefactive products in the gut. They also include substances such as indole and skatole, which are indicators of a deteriorating intestinal environment and are also described as putrefactive metabolites that cause the unpleasant odor of flatulence.
Thus, gut microbial metabolites affect our health, for better or for worse. One question naturally arose in our minds: do gut microbial metabolites also affect dementia? To answer this question, we obtained the cooperation of 107 patients, including 25 with dementia. We measured the concentration of 14 gut microbial metabolites in fecal samples we had collected, and then used clinical information to analyze the relationship between gut microbes and cognitive function.
To cut straight to the conclusion, we found that gut microbial metabolites were strongly associated with cognitive function (Figure 3). The feces of people with dementia contained high concentrations of metabolites produced by harmful microbes, such as ammonia, p-cresol, and indole. Conversely, hardly any such substances were found in people who did not have dementia. On the other hand, the metabolite that was abundant in people without dementia but not in dementia sufferers was lactic acid.
 Modified from Saji N, et al. Sci Rep, 10(1):8080, 2020.
Modified from Saji N, et al. Sci Rep, 10(1):8080, 2020.
Figure 3. Microbial metabolites and dementia
Odds ratio (95% confidence interval) for one SD increase in metabolite concentrationThe horizontal axis shows the association between gut microbial metabolites and dementia. The higher the figure for each metabolite, the more abundant it was in the feces of dementia sufferers and the less abundant it was in those without dementia, so there is thought to be an association with dementia.
From statistical analysis, we deduced that every one standard deviation (SD) rise in ammonia concentration was associated with around a 1.6-fold increased risk of dementia, while one SD rise in lactic acid concentration reduced the dementia risk to roughly 0.3-fold.
I will explain a little more about ammonia and lactic acid. Some metabolites are absorbed from the digestive tract and travel throughout the body in the blood via the circulatory system. Some studies have reported an increased risk of cognitive impairment or Alzheimer’s disease if the blood concentration of ammonia becomes too high. The lactic acid produced by beneficial bacteria curbs the proliferation of harmful microbes and boosts intestinal motility. Lactic acid is also known to create an intestinal environment that prevents infection by microbes capable of causing food poisoning and pathogenic microbes, and curbs the production of carcinogenic putrefactive products.
Increasing the proportion of beneficial bacteria in the gut microbiome is crucial to our physical health. It has now become apparent that boosting beneficial bacteria and reducing harmful microbes is also vital when it comes to the relationship between gut microbial metabolites and dementia.
Lifestyle habits and prevention of dementia
Patients and their family members whom I meet in the course of outpatient consultations often ask me whether there is a remedy for dementia. My answer is always the same: unfortunately, not at this stage. However, there are lifestyle habits that can assist in prevention. One of these is diet. The gut microbiome and gut microbial metabolites cannot be separated from diet.
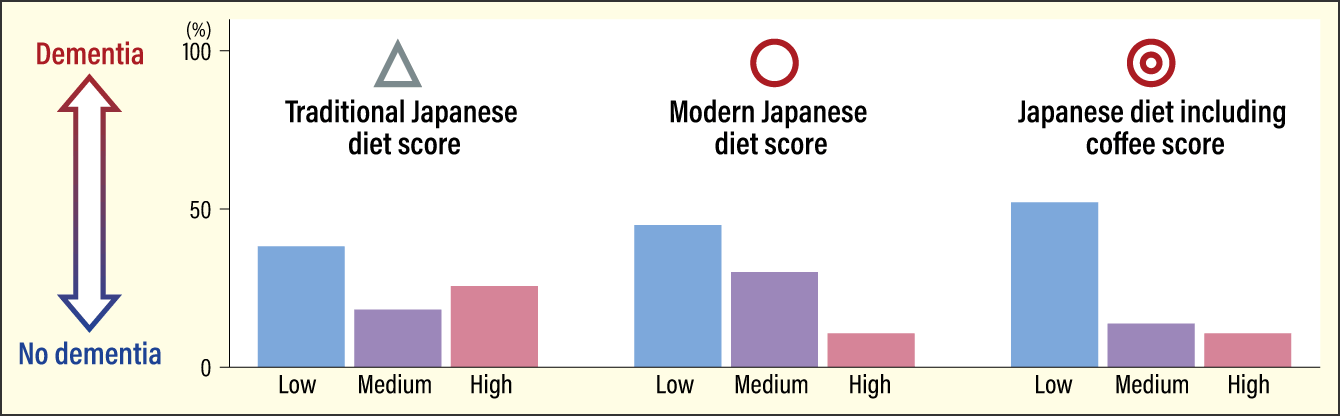
A Tohoku University cohort study that investigated the association between elderly people’s diet (with dietary patterns classified into three categories: Japanese pattern, animal food pattern, and high-dairy pattern) and dementia reported in 2016 that individuals whose diet scored higher for the Japanese pattern had a lower risk of dementia. So, which foods in Japanese cuisine should people eat to reduce dementia risk? With the cooperation of 85 patients, including 23 with dementia, we conducted a dietary questionnaire and investigated the relationship between a Japanese-style diet, the gut microbiota, and cognitive decline.
Worthy of mention is the fact that, in calculating the diet scores, we classified the dietary content for which points were assigned into three categories: the traditional Japanese diet, based on rice, miso, fish and shellfish, green and yellow vegetables, seaweed, pickles, and green tea; the modern Japanese diet, based on the aforementioned items, plus soybeans and soybean-derived foods, mushrooms, and fruit; and the Japanese diet including coffee, which includes all of the foregoing items, plus coffee.
There are studies from around the world that have shown coffee to have a beneficial impact on cognitive function. Social activities such as outings and interaction with friends are also related to the dementia risk assessments.
We calculated each person’s score from their questionnaire, then combined it with clinical information whether or not the individual had dementia, and analyzed the data. The following became apparent from our results: compared with dementia sufferers, people without dementia have a higher Japanese diet score, and consume larger amounts of fish and shellfish, mushrooms, soybeans and soybean-derived foods, and coffee. In addition, we saw a tendency for those who consume larger amounts of these foods to have a good intestinal environment, with lower concentrations of gut microbial metabolites. We concluded that adherence to a traditional Japanese diet was inversely associated with cognitive decline and tended to be associated with lower concentrations of gut microbial metabolites (Figure 4).
 Modified from Saji N, et al. Nutrition, 94:111524, 2022.
Modified from Saji N, et al. Nutrition, 94:111524, 2022.
Figure 4. Japanese diet and prevalence of dementiaThere was a higher prevalence of dementia among those in the low-scoring group for each of the three dietary patterns. Dementia was lowest among the group with high scores for Japanese diet including coffee. The content of our diet alters our intestinal environment. Switching to a Japanese diet including coffee may have the potential to prevent dementia in the future.
We are continuing to study gut microbes and dementia; aside from this set of research findings, we have also identified that gut microbes are associated with white matter hyperintensity and brain atrophy, and have found an association between lipopolysaccharides (components of bacteria) and mild cognitive impairment. There are various types of dementia besides Alzheimer’s dementia. Accordingly, we plan to start investigating the relationship between gut microbes and another type, Lewy body dementia. We are only part of the way along the long journey toward unraveling the detailed route of the gut–brain axis and shedding light on the mechanisms via which gut microbes are associated with dementia. There are hopes that this will lead to the development of dementia remedies.
A diet that increases beneficial gut microbes and gut microbial metabolites that are good for our health has the potential to help prevent dementia. We recommend that you rethink the content of your diet once you reach your 40s and strive to prevent dementia by regulating your intestinal environment.