Just like our vision and hearing, our sense of smell declines as we age. Annoyingly, unlike with our other senses, it can be hard to spot our olfaction failing and it is not something covered by routine medical examinations, either.
However, a diminished sense of smell poses various problems in daily life, from making meals less tasty to depriving a person of the ability to immediately detect hazards such as rotting food, gas leaks, and fires. Furthermore, scientists have discovered a relationship between a waning olfaction and conditions that pose a risk of dementia and various other diseases: frailty and sarcopenia. It is therefore desirable to spot a decline in the sense of smell as soon as possible, and to use this insight for the prevention and early detection of disease.
Special Feature 1 – The Science of Smell How maintaining the sense of smell can help prevent frailty and sarcopenia
composition by Yumi Ohuchi
illustration by Rokuhisa Chino
special thanks to Richard M. Costanzo (Virginia Commonwealth University)
Olfactory disorders have attracted attention of late as one of the aftereffects of COVID-19. Mainly caused by sinusitis or other diseases of the nose, olfactory disorders are characterized by subjective symptoms such as the complete inability to detect smells, everything smelling the same, or a change in the way things smell. Olfactory disorders can linger even after the symptoms of a cold or other viral infection of the upper respiratory tract have cleared up.
A diminished sense of smell poses problems in daily life
Our sense of smell declines as we age, just like our vision and hearing. However, unlike with those two senses, the failure of our olfaction function is hard for us to spot ourselves. In a study we conducted among healthy elderly people, more than 80% of respondents to our questionnaire reported that their sense of smell was normal, however when we performed olfactory testing of these same people we observed olfactory impairment in approximately 60%. Olfactory testing involved identifying 12 different odors highly familiar to Japanese people (Open Essence test); those who scored at least 8 out of a possible 12 points are deemed to have normal olfaction, while those scoring 7 or less are judged to have olfactory impairment. Some of those who thought their sense of smell was normal scored only 1 or 2 points, suggesting there are many hidden olfactory disorders that individuals suffering from them do not themselves notice.
Regardless of the presence or absence of subjective symptoms, a diminished sense of smell poses major problems in daily life, from making meals less tasty to depriving a person of the ability to detect hazards such as rotting food, gas leaks, and smoke from a fire. Furthermore, recent research has revealed that olfactory impairment not only reduces quality of life, but also is related to frailty (described in greater detail below), which increases the risk of dementia and various other diseases.
The link between olfactory impairment and the most common types of dementia —— Alzheimer’s dementia (AD) and Lewy body dementia —— was first highlighted several decades ago. There is also a connection to Parkinson’s disease, which is strongly associated with dementia. The relationship on which we should focus is that between mild cognitive impairment (MCI), which is the stage prior to AD, and olfactory impairment. Rather than being sudden in onset, AD progresses gradually; it is believed to develop following MCI, which manifests itself as symptoms including forgetfulness, depression, and anxiety. If treatment is started at the MCI stage, it might be possible to restore the patient to normal or to block the progression to AD.
For example, a prospective cohort study conducted in the U.S. among people with no decline in cognitive function reported that the five-year probability of developing MCI among elderly people with lower than average scores in odor identification tests is about 50% higher than among seniors whose scores were at or above the average.
- * Prospective cohort study: A research method that involves following a group of individuals (cohort) over time and observing the frequency with which a particular disease occurs among that cohort.
Using the smell of curry as an indicator
In another prospective cohort study in the U.S., focusing on patients with MCI, a combination of five predictors —— scores in a functional activities questionnaire, olfactory identification test, verbal memory test, MRI hippocampal volume, and MRI entorhinal cortex volume, which is linked to the sense of smell —— demonstrated that individuals with olfactory impairment showed a greater tendency toward progression from MCI to AD. The olfactory test used here involves identifying 40 different odors, with a maximum score of 40 points. Individuals who progressed from MCI to AD had a low score of 25.8 points on average out of 40 in the earlier test, while those who did not develop to AD were within the normal range, at 33.2 points on average.
From research reports of this kind, it is anticipated that olfactory impairment might serve as an indicator for the early detection of MCI. However, as stated above, many elderly people have an impaired sense of smell, even if they are healthy, and it is not the case that all of them will go on to develop dementia. It is therefore necessary to assess which elderly people with olfactory impairment are at high risk of MCI or of progression from MCI to AD.
Accordingly, we conducted a study of healthy seniors, MCI patients, and AD patients, using the Open Essence test. From the results, we discovered that the number of correct answers was highest among healthy seniors, followed by MCI patients, and then AD patients (Figure 1). Among AD patients, the extent of olfactory impairment was the same as that seen in patients with olfactory disorders who can hardly smell anything.
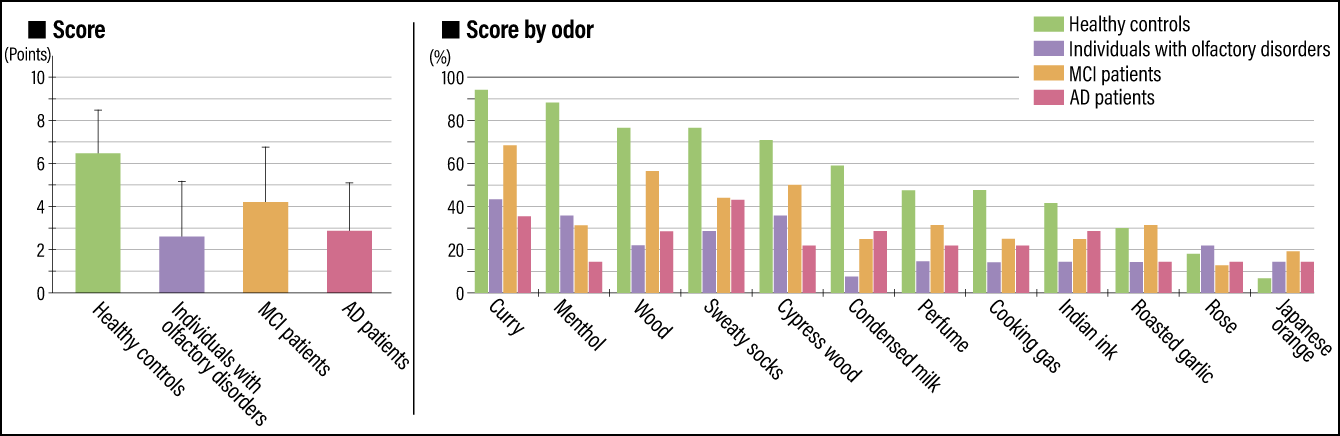
Figure 1. Results of the Open Essence test among healthy seniors, individuals with olfactory disorders, MCI patients, and AD patientsThere was little difference between AD patients and individuals diagnosed with olfactory disorders in terms of the score in the Open Essence test. The correct answer rate by odor suggested the possibility that the smell of curry could serve as an indicator for determining the risk of MCI or AD.
Furthermore, when looking at specific odors, we found almost all healthy seniors could identify the smell of curry, while only about 70% of MCI patients and around 35% of AD patients could smell curry. From this, we believe that the smell of curry could serve as an indicator for determining the risk of MCI or AD among Japanese people.
Along with dementia, frailty and sarcopenia among elderly people have come to be regarded as a problem in recent years. The term frailty describes a state in which physical, mental, and social debilitation and infirmity appear as mental and physical activity declines with age and vital functions are impaired, making the individual more prone to dementia, infectious diseases such as pneumonia, fractures, and joint disorders. Sarcopenia refers to reduced muscle mass and muscle weakness brought about by aging, causing gait disturbance and other forms of physical frailty. Physical frailty brings about social frailty by causing individuals to become housebound, which in turn leads to mental frailty, such as depression and dementia. Intervention is required at some stage to break this vicious circle.
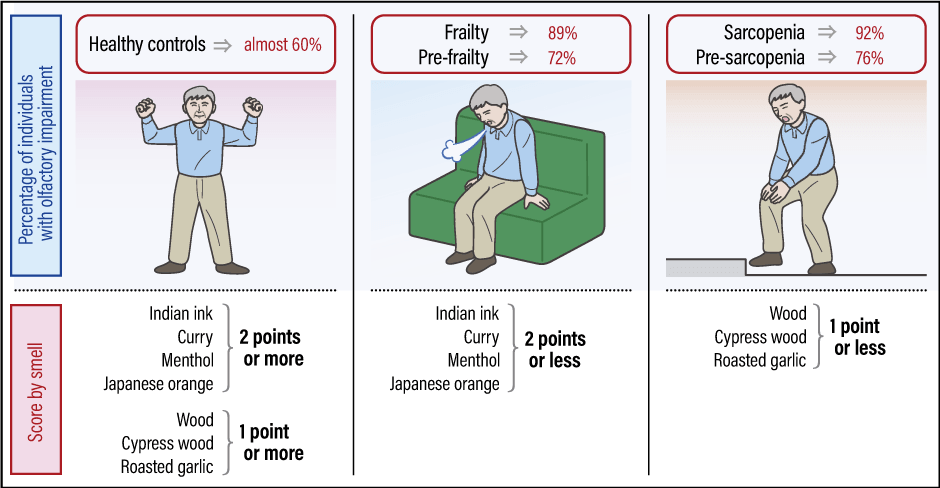
Olfactory impairment is thought to be a factor contributing to sarcopenia, as it leads to reduced appetite, thereby causing malnutrition. Accordingly, we conducted a study among 141 seniors aged 65 or above to investigate how olfactory impairment is connected to frailty and sarcopenia. We again used the Open Essence test for this study. Of the respondents, 13% demonstrated frailty and 35% pre-frailty, the prior stage, while 9% had sarcopenia and 29% pre-sarcopenia. Olfactory impairment was observed among 89% of respondents in the frailty subset, 72% in the pre-frailty subset, 92% in the sarcopenia subset, and 76% in the pre-sarcopenia subset (Figure 2). Although among healthy seniors, almost 60% were observed to have olfactory impairment, our study demonstrated that there was a statistically significant relationship between olfactory impairment, and frailty and sarcopenia, as well as the prior stages of frailty and sarcopenia.
 Compiled from Masayuki Harita, et al. Geriatr Gerontol Int, 19(5) :384-391, 2019.
Compiled from Masayuki Harita, et al. Geriatr Gerontol Int, 19(5) :384-391, 2019.
Figure 2. Relationship of olfactory impairment to frailty and sarcopeniaThere was also a higher proportion of individuals with olfactory impairment among those in the stage prior to developing frailty and sarcopenia than among healthy controls. In the score by smell, too, there were differences between healthy controls and individuals with frailty and sarcopenia, in terms of the smells they were unable to identify.
Smell influences loss of appetite more than taste
This study also examined the relationships of other diseases to frailty and sarcopenia, but we found no connection with lifestyle-related diseases such as diabetes, hypertension, and dyslipidemia. An unexpected result was that we found no link to frailty and sarcopenia in the case of taste disorders, which are thought to have the biggest impact on loss of appetite. In addition, this study used a questionnaire to investigate “flavor enjoyment” —— the ability to enjoy the taste of food —— and we found olfactory impairment to be more strongly associated with a decline in flavor enjoyment than gustatory impairment. When it comes to enjoying food, not only the taste, but also the flavor is important; the sense of taste —— that is to say, the functioning of the taste buds on the tongue —— does not decline with age to the same degree as the sense of smell. Accordingly, it is thought that a reduced sense of smell has more of an impact on loss of appetite than a waning sense of taste. Additionally, this study revealed a connection between a decline in flavor enjoyment and sarcopenia, because when the ability to enjoy flavors declines, so does appetite, along with other forms of interest in food, which in turn raises the risk of reduced activity levels, leading to sarcopenia.
We also found differences between healthy seniors and individuals with frailty and sarcopenia, in terms of the smells they were unable to identify. In those with sarcopenia and pre-sarcopenia, the total scores for wood, cypress wood, and roasted garlic were 1 point or less, while among those with frailty and pre-frailty, the total scores for Indian ink, curry, menthol, and Japanese orange were 2 points or less. Thus, the results of our analysis suggested the possibility that such scores were indicative of these states. In other words, just as with MCI and AD, it appears possible that the types of smell people are unable to identify could be indicators for the early detection of frailty and sarcopenia.
Many studies have also reported that olfactory impairment was associated with higher mortality. For example, in a prospective cohort study conducted among subjects aged 60 or above in Australia, the mortality rate over five years was 8.3% among those with normal olfaction, however it was 16.4% among those with mild olfactory impairment and 27.4% among those with moderate olfactory impairment, demonstrating that mortality increases with the degree of impairment. There is also a U.S. study showing that five-year mortality was around four times higher for older adults who had completely lost their sense of smell (anosmia), than for individuals with normal olfaction. In addition, this study demonstrated that mortality among anosmic individuals is higher than among those with heart failure, stroke, cancer, diabetes, or chronic obstructive pulmonary disease. These results are astonishing, showing that anosmia was a greater risk factor for death than conditions known to be leading causes of death. It is unclear why anosmia is associated with mortality, but conditions such as dementia and frailty are presumed to be involved.
Another study in the U.S. found that 15-year survival rates among individuals with a sensory impairment affecting either their hearing, visual acuity, or olfaction were lower than among individuals with no such impairments, and lower still among those with two or more of the sensory impairments in question. This report also demonstrates that olfactory impairment was most strongly associated with a decline in survival rates. Although the reasons for these results are unclear, it could conceivably be related to the fact that, whereas reduced visual acuity can be corrected with spectacles and hearing impairment with hearing aids, there are no assistive devices to compensate for olfactory impairment.
Olfactory impairment as a sign of disease
The reasons why these phenomena related to olfactory impairment occur have not yet come to light. However, the important thing is that, as described above, olfactory impairment could potentially be an indicator for the early detection of dementia, frailty, and sarcopenia (Figure 3). In our clinic, we undertake thorough examinations of elderly people with olfactory disorders of unknown cause, performing MRIs of the brain to measure the volume of the olfactory bulb, which processes information about smells. When we suspect MCI or AD, we use MRI software that measures the volume of areas of the brain demonstrating atrophy characteristic of AD at our university hospital’s Dementia Center.
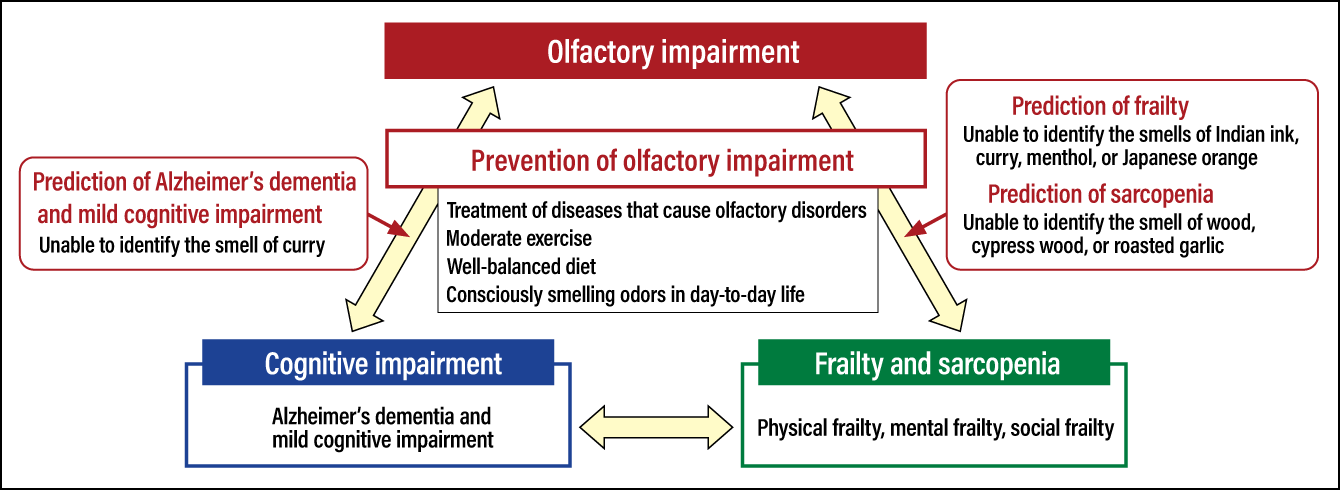
Figure 3. Relationship between olfactory impairment, cognitive impairment, and frailty/sarcopeniaOlfactory impairment could potentially be an indicator for the early detection of cognitive impairment, frailty, and sarcopenia. Moreover, preventing olfactory impairment could help to prevent these diseases.
It is also thought that maintaining the sense of smell could help to prevent associated diseases. To prevent olfactory impairment, it is vital to properly diagnose and treat any nasal diseases that could cause olfactory disorders. Smoking and lifestyle-related diseases such as arteriosclerosis and diabetes are known risk factors for olfactory impairment. This means that a balanced diet and moderate exercise are important. There are research reports showing that doing sufficient exercise to break a sweat at least three times per week prevents olfactory impairment. Our study showed that men with normal olfaction often ate dairy products. Foods that have a positive effect on the sense of smell in this way are a very interesting topic for consideration.
It is also crucial to consciously smell odors and think about what the smell is. Olfactory training, which involves smelling lemon and three other odors in the morning and evening, was developed in Germany as a treatment for olfactory disorders. Believed to promote the regeneration of olfactory sensory neurons, stimulation of the nasal mucosa has proven highly effective in achieving improvements. Making a habit of consciously smelling odors also provides an opportunity to notice any deterioration in olfaction.
Advances are now being made in the treatment of olfactory disorders. While the most important thing is to treat the primary disease, a traditional Chinese medicine called Dang Gui Shao Yao San, which is made with Angelica sinensis and Chinese peony, has been demonstrated to be highly effective against olfactory disorders following colds and brain trauma. Dang Gui Shao Yao San activates the nerve growth factor, and our research has shown that this nerve growth factor is involved in the regeneration of olfactory sensory neurons. At our outpatient clinic dealing with olfactory disorders, we are also considering an approach based on the aforementioned olfactory training that is suited to Japanese people.
The sense of smell tends to be disregarded; for example, it is not included in routine medical examinations. The Open Essence test we used in our studies can easily be administered, but at present it is used only for research purposes and the costs are borne by the medical institution. With the super-aging of Japanese society set to escalate further, I believe it is important to raise interest in the sense of smell among the public, in order to increase opportunities to spot olfactory impairment to ensure the early detection and prevention of a variety of diseases.