The onset of dementia involves various conditions, such as genes and sex hormones, and its precise mechanism has not been clarified. However, it has been known among medical workers that there are differences between men and women, or sex differences, in dementia. The incidence of Alzheimer’s disease in women is about twice that in men, and they account for a larger number of patients than men. Nursing care workers have come to recognize diversity in sex, and be more aware of considerations to sexual minorities.
Special Feature 1 – Diversity in Sex Medical and nursing care for dementia patients with consideration of sex differences
text by Toshiko Mogi
The article Ninchi-shō to Seisa (Dementia and sex differences) published in 2017 received a great response. The lead author, Dr. Ryo Kumagai, is not a researcher specializing in gender-specific medicine, as he encountered many patients with dementia as a clinical psychiatrist, he realized that more women than men developed dementia, particularly Alzheimer’s disease.
Dr. Kumagai said:
“For more than ten years, I have gained clinical experience that new patients ‘after menopause’ who have ‘diabetes’ but have not made regular visits to a hospital are more likely to have Alzheimer’s disease than a psychiatric disease such as schizophrenia. I believe that this experience-based awareness is not only mine, but is shared by many clinical psychiatrists.”
Dementia collectively refers to a state in which cognitive functions (thinking, memory, and logical reasoning) decline to a level that interferes with daily or social activities due to various causes, and it is classified into several types. The most common type, constituting about 60% of the total, is Alzheimer’s disease. The next is vascular dementia, followed by Lewy body dementia, frontotemporal dementia, and others. Among such various types of dementia, the incidence of the Alzheimer’s disease is said to be high in women.
“Alzheimer’s disease is considered to develop as a result of unnecessary amyloid beta and tau protein accumulating in the brain over a long period of more than ten years, and the entire brain, mainly the hippocampus which controls memory, shrinks due to brain cell damage or the decrease in neurotransmitter levels (Figure 1).
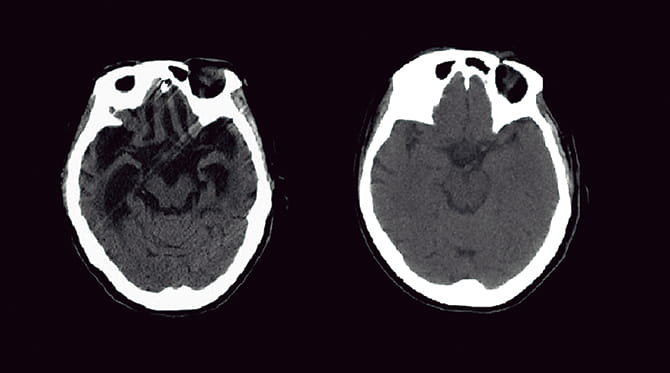
Figure 1. Brain shrinkage in Alzheimer’s disease shown in comparative imagesBoth images are computed tomography (CT) scans of the heads of women in their 60s (left: the brain of a patient with Alzheimer’s disease; right: a normal brain). In Alzheimer’s disease, shrinkage is observed in the entire brain, mainly in the hippocampus.
In addition to this basic outline, the onset involves various conditions, such as genes and sex hormones. My personal view is that there are various factors including those that have yet to be elucidated, and the onset is triggered when all of the required conditions are met.”
Dr. Kumagai says that, when he was considering the conditions for the trigger from several keywords such as women, genes, and sex hormones, the term “sex differences” emerged. I asked him about sex differences concerning dementia in medical and nursing care, which he found while treating and studying patients with dementia.
Aging is one of the greatest risk factors for the onset of dementia. It is clear from international comparison of that life expectancy at birth Japan has one of the longest life expectancies in the world. According to the ”Abridged Life Tables for Japan” (2018) released by the Ministry of Health, Labour and Welfare (MHLW) in 2019, life expectancy at birth was 81.25 years for males and 87.32 years for females, both marking a record high (males: 81.09 years, females: 87.26 years in 2017) (Table 1).
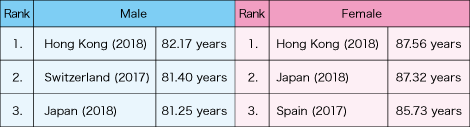
Table 1. International comparison by life expectancy at birthAccording to the MHLW, life expectancy at birth in Japan marked a record high both for men and women in 2018, and the number of people aged 100 or over exceeded 70,000. Because of this, both men and women rank in the world’s top three countries by life expectancy at birth.
(Source: MHLW, “Overview of 2018 Abridged Life Tables for Japan”)
Background to the higher incidence of Alzheimer’s disease in women
Statistics by the Ministry of Internal Affairs and Communications (MIC) show that, as of September 2018, the population aged 65 and over was 15.45 million males and 20.12 million females, with the female elderly population exceeding 20 million for the first time. While the male population is larger in the age group of 15-64 years, the female population outnumbers the male population in the age group of 65 years and over.
As women have a longer average life expectancy than men, and their proportion in the elderly population is relatively larger than men, it is understandable that there are more women with dementia associated with aging than men. As the Alzheimer’s type is the most common dementia, we can derive the high prevalence of the disease among elderly women.
“There also were more female inpatients in a geriatric ward where I used to work (Table 2). However, there have been many reports that, even if the differences in population or longevity were statistically excluded, women are still more susceptible to developing Alzheimer’s disease. It is considered that factors other than aging also trigger the onset of the disease in women.”
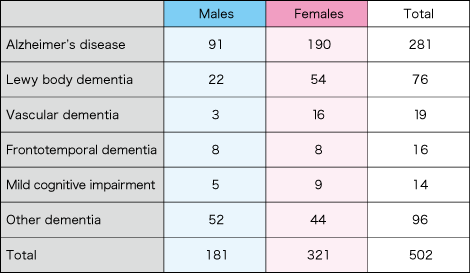
Table 2. Breakdown of new inpatients to the dementia ward of a geriatric hospital in Tokyo in 2018The number of female patients outnumbered that of male patients for all items, including the total number of inpatients in the dementia ward. For Alzheimer’s disease, the number of female patients was slightly over twice the number of male patients.
(Surveyed by Ryo Kumagai)
One of the key factors is diabetes. The blood glucose level is controlled by insulin secreted from the pancreas. Used insulin and for the brain unnecessary amyloid beta are degraded by an insulin-degrading enzyme (IDE). If the hyperglycemia state continues and the amount of insulin secretion increases, IDE can no longer degrade amyloid beta, and hyperglycemia also damages blood vessels throughout the body, including the brain. From the medical perspective, it is considered that a complex set of conditions caused by hyperglycemia lead to Alzheimer’s disease. While there is no major difference between men and women in the number of patients with diabetes, the percentage of outpatients is lower in women than in men.
“There is no clear evidence linking all of these factors. However, we assume that these combined conditions account for the fact that a large proportion of female patients with Alzheimer’s disease also have diabetes.”
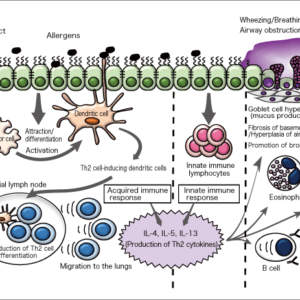
When thinking about sex differences in diseases, the effects of female sex hormones cannot be ignored. Estrogen functions to maintain the mental and physical health in women.
“Estrogen also performs important functions in the brain. There are estrogen receptors in the brain, and estrogen works to enhance the neural synaptic function or suppress neuronal cell death by amyloid beta.”
In perimenopause, the activity of the ovaries declines, and the level of estrogen secreted from the ovaries drops sharply.
“This is considered to have an adverse effect on the brain functions and increase the onset risk of Alzheimer’s disease.”
One of the therapies for treating climacteric symptoms and disorders is hormone replacement therapy (HRT), which supplements the estrogen lacking in the body during perimenopause. Based on the hypothesis that the postmenopausal decline in estrogen levels is associated with the onset of Alzheimer’s disease, many studies have been conducted to explore the possibility of using HRT for preventing the onset of the disease.
“Simply put, the results of such studies show that the onset risk of Alzheimer’s disease declines by administering estrogen immediately after menopause. However, if estrogen is administered a long time after menopause, particularly at old age, the risk increases instead. The results also differ according to the duration of therapy, so HRT seems to be effective under limited conditions.”
Although many aspects have yet to be clarified, Dr. Kumagai confirms the fact that the therapy had some effects on reducing the onset risk.
Sex differences in symptoms and nursing care
Let us look at sex differences after the onset of dementia. There are cases in which the deposition of amyloid beta in the brain and brain shrinkage can be observed in inspection images, but no dementia symptoms are present, or in which the symptoms are less severe as compared to the level of brain shrinkage. This is thought to be due to a cognitive reserve, which is also subject to sex differences.
Cognitive reserve is a function of the brain which can compensate for damage caused to brain functions. The levels of cognitive reserve differ depending on levels of intellectual functions acquired through educational or occupational attainments before the brain damage occurred. Due to the effect of gender norms and other factors, the cognitive reserve is considered to be higher in men than in women in the case of the elderly. There also are reports that men have larger brains than women.
“Although men show stronger brain shrinkage, their scores in cognitive assessments are about the same as women’s scores. It is considered that the cognitive reserve contributes to less severe symptoms compared to the degree of actual brain damage.” (Figure 2)
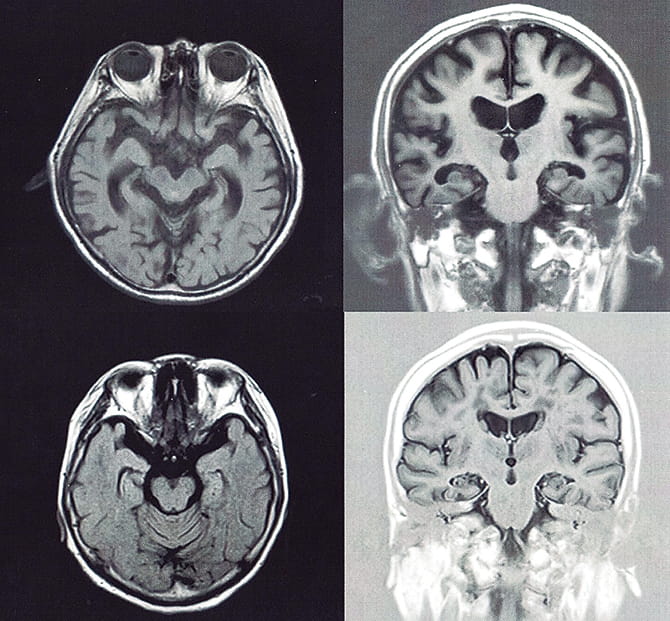
Figure 2. Sex differences in cognitive reserveThe images are magnetic resonance imaging (MRI) scans of the heads of patients with mild dementia (two upper images: a man aged 85; two lower images: a woman aged 72). The scores in the cognitive assessment called “mini-mental state examination” (MMSE) were 21 for the man and 20 for the woman. In this 30-point-scale assessment, 21 or below is judged to be “rather strongly suspected of dementia.”
The main symptoms of dementia can be largely divided into core symptoms and behavioral and psychological symptoms of dementia (BPSD).
Core symptoms are directly caused by brain damage, such as memory disorders (forgetting past experiences and being unable to memorize new things) and disorientation (becoming confused about time or a person in front of you). These symptoms occur in almost all patients that develop dementia.
The BPSD comprises psychological symptoms such as anxiety, depression and delusion, and behavioral symptoms such as wandering, violence and verbal abuse. They occur on the basis of core symptoms, due to the effects of the individual’s physical environmental and psychological factors.
Dr. Kumagai says sex differences can be found in these symptoms as well.
“While women are said to inherently have strong anxiety and depression, there is a report that they also often suffer from persecutory delusions, which is one of the BPSD phenomena. In the case of men, aggressiveness and violence against caregivers often become an issue.”
Symptoms are diverse, and this often imposes a burden on caregivers. Let us cast our eye to the nursing care environment, where we can also observe sex differences.
Looking at the main causes for requiring nursing care in the “Annual Report on the Ageing Society” (2018), “dementia” accounted for the highest proportion at 18.7%. Asked about the person who he/she wants to receive care from, the most common answer was “spouse” for males at 56.9% and “home-care worker/long term care service staff” for females at 39.5%.
In cases of actually receiving nursing care, the principal caregivers are family members (such as spouse, children, or children’s spouse). Such family members are males in 34.0% and females in 66.0% of cases. The spouse is a caregiver in 25.2% of cases, and there seems to be a considerable number of cases in which one elderly person gives care to another (referred to as “rō-rō kaigo” in Japanese).
These data reflect the reality that there are a larger number of patients with dementia among women on the one hand, but women are the main caregivers on the other hand. Therefore, cases of “rō-rō kaigo” are likely to include cases where one elderly person with dementia gives care to another with dementia (referred to as “nin-nin kaigo” in Japanese).
Sex differences in role sharing may be more correctly defined as socially and culturally created gender differences, rather than biological sex differences. Nevertheless, such differences affect the quality of nursing care at home.
“When a man becomes a caregiver, be it a spouse or child, the quality of care may be lower than in the case of a female caregiver, due to being unfamiliar with housework or being a little crude physically or verbally because of the conventional gender norms.”
Future challenges including response to LGBT
Sex differences in dementia are also related to the quality of care provided at medical and nursing facilities. At present, these facilities give care to patients conventionally divided by “physical sex” based on the biological definition. For example, in an inpatient ward, patients of the same sex are to share the same multiple-bed room in principle, such as male patients in one room and female patients in another. In addition, most of the facilities position caregivers of the same sex as the patients, in order not to impair their dignity when they are assisted in bathing and excretion-situations that may easily cause the patients’ embarrassment.
However, it has been gradually recognized that sex is diverse. In recent years, we have increasingly heard the term “LGBT” in news reports, etc. LGBT is a term that represents sexual minorities, taking the initial letters of lesbian, gay, bisexual, and transgender.
“There are sexual minorities among elderly as well recently, or rather, they must have been there for long time. According to literature, they have been treated individually as special cases. Today, instead of treating them as special cases, it is necessary to study what kind of consideration should be given to sexual minorities in medical and nursing care to provide them with better care.”
Many transgender people have physically changed their body through surgery to match their identified gender. Some people who have changed their body from male to female continuously take female sex hormones in order to maintain a rounded, feminine body. While there are many reports on the relationship between female sex hormones and dementia there are too few case studies on sexual minorities.
“Also lacking are methods of medical treatment and nursing care plans like day care service for elderly male patients with dementia. This may be because the absolute number of such patients is small. I consider the response to such patients, including the response to LGBT, to be future challenges that must be addressed from the viewpoint of improving the quality of care for dementia patients.”
Lastly, I asked a question that had been bothering me. Are there also sex differences in prevention of dementia?
“Being a woman is said to be the greatest risk for Alzheimer’s disease. However, you do not have to give up just because you are a woman. In order to extend a healthy life expectancy, a healthy diet and moderate exercise to avoid lifestyle-related diseases are essential. There are no sex differences in prevention.”
As stimulation for activating our brains, he advises that we should try to have many occasions to feel “delight” and “pleasure” among the major emotions (delight, anger, sorrow, and pleasure) in our daily lives. Tasty, fun, happy-we should lead a life filled with such feelings.